Integrated Analysis of Laparoscopic Training – A Data-Driven Approach
Our simulators use advanced algorithms to evaluate training sessions, offering clear feedback on what went well and what needs refinement. After each session, trainees receive a detailed report that analyzes their technique, highlights mistakes, and suggests ways to improve.
Laparoscopic training is most effective when paired with detailed debriefing. Studies have consistently shown that debriefing is an essential part of surgical education, helping trainees reflect on their performance, identify mistakes, and refine their techniques. Structured feedback has been linked to improved skill retention, fewer errors, and better overall competency. That’s why our simulators provide a comprehensive training summary after every session. This feedback loop doesn’t just track completion – it ensures trainees understand their strengths and pinpoint areas for improvement, ultimately leading to safer and more efficient surgical practices.
How It Works
Our simulators use advanced algorithms to evaluate training sessions, offering clear feedback on what went well and what needs refinement. After each session, trainees receive a detailed report that analyzes their technique, highlights mistakes, and suggests ways to improve.
Our approach is continuously validated through feedback from experienced surgeons, residents, and trainees at different skill levels. Training scenarios are repeated multiple times to collect reliable data, ensuring the guidance provided is both accurate and practical.
Training Results: Pass or Fail?
Each training session is evaluated based on a set of objective criteria to provide a clear result for the trainee:
- Pass: The trainee meets all necessary benchmarks and can either move on to the next challenge or repeat the session for further improvement.
- Fail: Critical safety or technical benchmarks were not met, requiring the trainee to redo the exercise.
The evaluation is based on three key components:
- Training Execution – Did the trainee follow the scenario instructions?
- Motion Parameters – Were the instruments handled efficiently and safely?
- Intraoperative Events – Were there any major events detected?
Training Execution
Correct execution is crucial for valid assessments. If a trainee deviates from the required steps, results from other evaluation criteria become unreliable. To ensure proper execution, we use:
- Automatic step verification – Our Laparo Apex and Laparo Apex PRO simulators detect whether the trainee performed all necessary steps correctly in virtual guided scenarios.
- Video comparison – The trainee can review their session alongside a tutorial video to self-assess their performance.
- Instructor assessment – Supervisors can manually review training records and adjust outcomes if necessary.
Motion Analysis Parameters
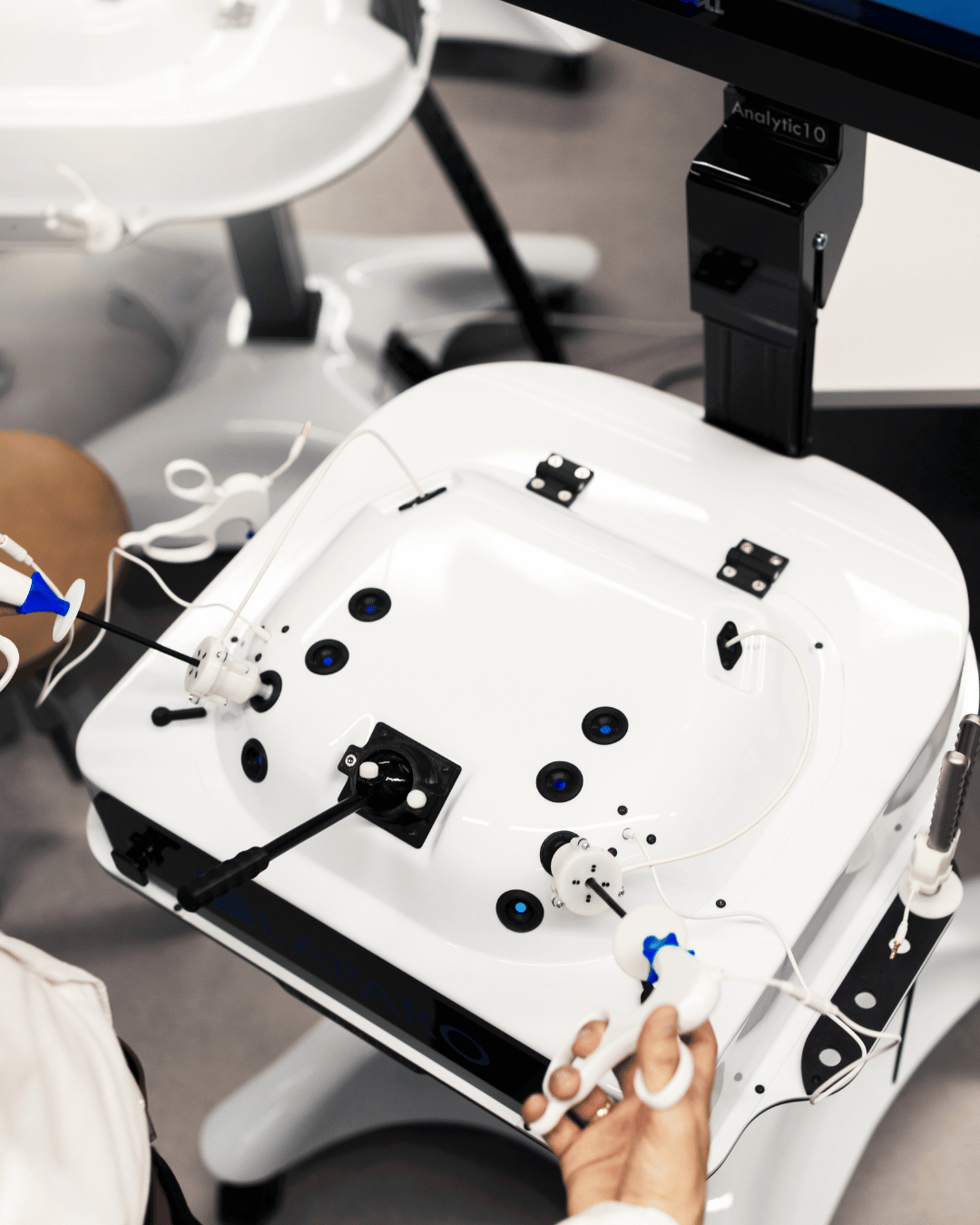
Our simulators are equipped with real-time motion tracking and precise sensors to collect movement data from instruments. This data is used to assess performance based on established research in surgical training.
Motion analysis serves two main purposes:
- Ensuring Patient Safety – Our system detects risky motion patterns, such as sudden movements, excessive acceleration, or instrument activity out of view. These factors are linked to increased surgical errors. By setting limits on these variables, we ensure trainees develop safe habits. Exceeding these limits results in a failed session, requiring further practice.
- Tracking Skill Progression – Mastery of laparoscopic surgery is about refining technique over time. Our motion tracking records data across sessions, helping trainees measure improvements in efficiency, precision, and control. Key parameters such as time, path length, or economy of volume provide insight into performance trends.
Additionally, some parameters act as extra validation tools. If achieved values fall significantly outside expected limits, the session may be deemed invalid to maintain consistency in evaluation.
Key Motion Parameters
Time: Measures the total session duration. Experts complete tasks faster, but we do not encourage novices to rush – speed is expected to improve naturally with experience. Research shows shorter operative times are linked to better patient outcomes and lower complication risks.
Path Length: Tracks the total distance traveled by the instrument tip. Shorter path length indicates greater efficiency, as excessive movement can increase tissue handling and prolong the procedure. Novices often take longer, less direct routes due to hesitation or lack of precision. Over time, training helps refine movements, reducing unnecessary motions and enhancing overall procedural efficiency.
Number of Openings/Closings: Counts how often the instrument jaws are fully opened and closed. Experts demonstrate more controlled grasping behavior, minimizing unnecessary or excessive movements. This skill is crucial because improper grasping can lead to tissue damage or inefficient handling of surgical tools.
Idleness: Measures how much time the instrument remains stationary. While brief pauses can indicate careful decision-making, excessive idleness may reflect hesitation or lack of confidence. Experts maintain a smooth and continuous workflow, minimizing unnecessary downtime.
Excessive Speed & Acceleration: Detects sudden, uncontrolled movements, which can be dangerous. A speed limit is set to prevent abrupt, uncontrolled actions that could harm tissue. Experienced surgeons achieve high efficiency without unnecessary force, while novices may struggle with overcompensation or unsteady hands. Developing controlled and deliberate movements is key to safe and effective surgical performance.
Bumps: Measure how often instruments hit each other or other solid objects. Unintentional collisions can result in tissue damage or disrupt the surgical workflow. Avoiding instrument bumps requires good spatial awareness and hand-eye coordination, which improve with training.
Visibility parameters track unsafe activity outside the view of the camera:
- Time out of sight tracks how long the instrument tip is outside the field of view.
- Movements out of sight tracks the total distance the instrument travels while outside the visible area. This is crucial because long movements out of sight indicate poor spatial awareness and a higher likelihood of accidental damage.
- Openings/closings out of sight counts how often the instrument jaws are operated while the tip is not visible. This parameter highlights unsafe practices, as manipulating tissue blindly can lead to unintended injuries.
Bimanual Dexterity measures coordination between the left and right hands. High dexterity correlates with improved surgical precision and efficiency. Effective use of both hands reduces procedure time and enhances surgical control.
Economy of Area & Economy of Volume evaluate how efficiently the trainee uses the available workspace. Experts operate within a controlled, minimized space to reduce unnecessary motion. Training develops an understanding of optimal instrument positioning and movement efficiency.
Motion Smoothness assesses fluidity and steadiness of instrument movements. Smoother movements correlate with expertise and reduced risk of unintended injury, while hesitant or jerky movements can lead to errors.
Depth Perception measures how effectively the trainee perceives depth and distance. This skill is essential for precise movements and avoiding tissue damage.
Motion Analysis Module
Our Motion Analysis Module is a key component of our simulators, responsible for calculating Motion Analysis Parameters (MAPs) in real time. For research institutions, we offer free access to this module to support advancements in surgical education.
The module is built on validated algorithms derived from the latest research, ensuring high accuracy and relevance. It can be used as a standalone tool for research purposes, and users can customize or extend the algorithms to fit their specific needs. Detailed documentation and tutorials are available for seamless integration into research projects.
Contact us for more details.
Intraoperative Events
Our virtual scenarios analyze interactions between laparoscopic instruments and tissues and monitor tissue state in real-time. We analyze factors such as force applied to tissue, improper electrosurgery activations, and any unintentional trauma caused by excessive pressure or poor technique. We track intraoperative events in real-time, providing trainees with immediate feedback on potential errors and their impact. Each event is detailed, allowing the trainee to understand exactly which organ was affected, what type of injury occurred, and the potential consequences of such an error.
Categorization of Intraoperative Events
Major intraoperative adverse events ( iAEs) – These indicate life-threatening surgical risks and result in an automatic failure of the session. They include severe tissue damage, accidental perforations, and excessive bleeding. These events represent the most critical mistakes, as they pose an immediate threat to patient survival. The system provides detailed feedback on the type of injury, the affected organ, and the potential consequences, ensuring that trainees understand the severity of their errors and how to avoid them in future procedures.
iAEs (Non-Life-Threatening Adverse Events) – These events do not pose an immediate threat to the patient’s life but can still impact patient recovery and post-operative outcomes. While not as critical as major iAEs, these errors should be corrected to ensure optimal patient outcomes.
Suggestions (Bad Habits) – These are flagged when suboptimal techniques are observed that do not directly impact patient safety but could lead to inefficiencies or increased risk over time. Examples include unnecessary not recommended clipping order or too long electrosurgery activation. These habits are highlighted in the performance review, allowing trainees to refine their technique progressively without immediate failure consequences.
Notes
Notes help both trainees and instructors keep track of observations and feedback during training. Trainees can review their performance, while instructors can offer guidance or point out mistakes. Each note can be pinned to a specific moment in the session, making it easy to reference key actions or behaviors. This makes feedback more precise by tying comments directly to relevant moments. Plus, trainees can jump straight to the corresponding part of their recorded session with a single click, making the review process smooth and efficient.
Final Thoughts
With our training summary module, we combine real-time motion tracking, performance metrics, and defined safety parameters to offer trainees a structured and data-driven approach to laparoscopic training debriefing.
This system is designed to:
✅ Identify and eliminate unsafe behaviors
✅ Track skill improvement over time
✅ Provide objective performance insights
✅ Help trainees develop efficiency while maintaining safe practices
By continuously refining our analysis methods, we ensure that each training session provides meaningful feedback, guiding trainees toward improved precision, confidence, and surgical proficiency.

